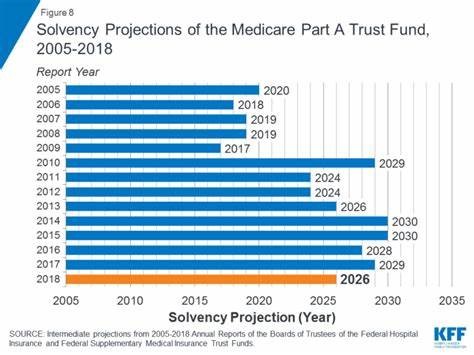
Healthcare benefits have taken a center stage on the national scene with presidential candidates proposing single-payer systems, improvements to Medicare benefits, additional cuts or increases to Medicaid and Medicare, and other scenarios. Many have leveraged the ever-changing statistic of when “Medicare will run out of money” as demonstrated by the graphic below.
Medicare and Medicaid consume large percentages of the federal budget. According to the Congressional budget office, in 2019 Medicare and Medicaid spending account for 14.4% and 9.2% of the federal outlay respectively. When a quarter of every dollar that the government spends is on healthcare, it is a big topic.
Federal budgets are not the only concern however, as states also have a role here. In the United States, individuals who are considered “dual-eligible” (qualifying for both Medicare and Medicaid benefits) consume, on average, 35% of state budgets. This portion of our population qualify for taxpayer-funded healthcare benefits either because of age, income, or disability and are often among the most medically fragile.
Medicare constitutes one out of every five dollars spent on healthcare in the U.S., with just 10% of Medicare beneficiaries using 60% of the money. Overall, the cost of the program continues to rise at an alarming pace. In 2008, we spent $525 billion on Medicare and just over 10 years later we are spending almost $700 billion. This 33% increase is concerning, given that we are on the edge of the largest wave of our population getting to the age where they will start consuming dollars quickly.
The issue is also not one of just dollars and sense, it is also about our overall health. We may be living longer but we are facing more illness and disease. For example, one out of three aging adults will face some loss of memory. By 2040, 14 million Americans will have dementia. According to the CDC, 78% of adults over the age of 55 have a chronic disease! And, nearly 50% have two or more and nearly 20% have three or more chronic diseases. In the graph below, you can see how healthcare spending rises dramatically with the addition of one or more chronic diseases.
What can be done?
Undoubtedly, those responsible for designing benefits and approaches to care have these statistics in mind, too. We see this reflected in the continued enhancements and push to use Medicare Advantage (MA) plans or Part C, which include incentives for private companies to assume the risk and management of these populations. The Centers for Medicare & Medicaid Services (CMS) have issued increased incentives for MA plans to specifically target those with chronic illness who require assistance with activities of daily living (ADLs), like walking, feeding, toileting, bathing, transferring, and grooming. Moreover, an effort is underway to add Home Care as a benefit available for purchase in Medi-Gap plans (insurance products designed to address healthcare expenses not traditionally covered by Medicare’s base benefits). CMS is incentivizing the development of best practices and innovation to address some of the rising needs of the aging and chronic condition population, as a way to provide better care and drive down cost.
Home Care cannot fix all the issues within our healthcare system. However, strong evidence demonstrates Home Care’s ability to dramatically reduce costs by preventing expensive medical interventions like Emergency Room visits and hospital stays. Home Care also can positively impact the social determinants of health that are strong predictors of outcomes or disease management by providing transportation, nutrition, reminders, and even companionship. When we develop a care plan for our clients, each plan specifically addresses the unique needs of that client. The plan may include intervention and assistance with managing ADLs and chronic illness to drive better compliance with treatment plans and prevent exacerbation of symptoms that often occurs when older adults are isolated.
The Home Care industry is working diligently to quantify the impact of our services and further study data about our contributions to reductions in healthcare spending and improved outcomes. Family Resource is busy positioning itself to be a leader in this data analysis. Our intent is to provide empirical proof behind the savings and outcomes that we already know we achieve on behalf of our clients and as a whole. This process is just one more way that we are advancing our mission of improving the quality of life for those we serve while being leaders in home care.






